About Care from the Oustanding Society
Sophie Chester-Glyn • 2 October 2019
Today was an outstanding day, not simply because the deluge of April showers in October disappeared, but because we were lucky enough to attend the Outstanding Society Network
event. This is our summary of some excellent talks and insightful messages from CQC, Care England, Alzheimer’s Society
and Wendy Mitchell.
Intro
The Care Quality Commission
carries out regular inspections of care services to make sure they are safe, caring, well-led, effective and responsive to people’s needs. Services receive a rating depending on the outcome of the CQC’s rating. The highest rating is an Outstanding one. The Outstanding Society is the brainchild of Camilla Trimble
who, whilst out walking her dogs, had a light-bulb moment and thought that there should be a forum for providers to share good practice in outstanding care services. With the help of Care England and Skills for Care, this has now grown into the Outstanding Society which shares best practice and meets annually to hear from health and social care leaders.
Coproduce Care is passionate about sharing the great things going on in care which many would not otherwise learn about. Therefore, feeling very fortunate to have been invited to the forum meeting this year (our director is part of a service rated outstanding by CQC), we are sharing some of the positive messages from today’s meeting.
(Whilst we are a big fan of the amazing Professor Martin Green
we opted to take the off-peak train to London and missed his talk at the start. However, all is not lost! We will be having a 1:1 with him later this year and sharing this on YouTube)
Avnish Goyal, Chair of Care England, gave an interesting session on the issues currently facing care. He questioned the claim, which some make, that we cannot fund social care. He also showed caution around the arguments to nationalise care. For Avnish, this would not necessarily take away the cost of care, but would take away the choice currently open to people in terms of service providers. In terms of long-term planning for social care, he called for a 30-year plan and an increase in the minimum wage as well as making planning easier so that services can be developed and managed in a more efficient way. An interesting point put forward was whether we should have a Commissioner for Older People.
Skills for Care Update
As hosts of the event, Skills for Care gave their own update. As many may or may not know, Skills for Care is the strategic body for workforce development in adult social care in England i.e. the social care version of Skills for Health and is on the lookout for a new CEO. This should be announced sometime in the Winter.
Skills for Care is also working on some very helpful guides for social care including effective supervision, time management and safety in social care. They have worked on these very coproductively with providers. An exciting development is a series of films coming out in spring 2020 to explore Outstanding organisations in different services such as residential, shared lives and homecare.
A message from Skills for Care to providers
Don’t forget, there is some very helpful
Workforce Development Funding (WDF), which is especially useful for some innovate courses run by Skills for Care such as a ‘Well-Led programme being rolled out which includes three one-day courses covering some of the core issues managers struggle with. Check out their
website for more.
Dementia experience from Wendy Mitchell ‘somebody I used to know’
Next came a tear-jerking session from the legendary Wendy Mitchell who was diagnosed with early dementia in her 50's. Wendy has used her experience of dementia to write a book
and share those experiences so that loved ones, carers and others can truly empathise with what some dementia sufferers experience. Here are some snippets from her talk today:
- If you notice some confusing frisking of a large wall mounted TV when it’s turned off, consider that it might appear as a hole in the wall to some dementia suffers – reflect on whether it should be covered up in some way.
- Never underestimate the benefits of Alexa: Wendy used it to remind her of things via her iPad when she was out and about, or to turn on the lights upstairs before she went to bed or simply to turn on some calming music when things were becoming overwhelming.
- Answering the phone seems such a natural thing to do, but for Wendy, people’s impatience whilst she thinks of her reply to questions they may ask, makes phone calls unbearable. She points out that ‘people can’t see you thinking on a phone call’. Therefore, she uses the more advanced mode of communicating with her family via FaceTime. She points out that having this different way of communicating makes it more apparent how heavily the NHS rely on telephone calls as their mode of communicating with patients.
- Fundamentally for Wendy, getting a diagnosis was a relief. It was the uncertainty of not knowing what was wrong before that, which made her life stressful. She had contemplated whether she had a brain tumour, or even worse. Getting the diagnosis meant she could move on with her life, although she had a few comments on how diagnoses could be announced to patients in more positive and humane ways.
We are definitely itching to read her book. If the book is anything like the person it will be interesting, emotive and enriching. Access it here. Wendy also writes a daily blog called ‘which me am I today?’
Jeremy Hughes – Alzheimer’s Society
A very impassioned Jeremy from the Alzheimer’s society
came next. The Alzheimer’s society is the UK's leading dementia support and research charity. Jeremy explained to us some of the fantastic things they are doing.
Firstly, he commended the care sector ball
which is held annually and aims to reward and recognise some of the great care carried out by people every day.
Jeremy went through the Alzheimer's Society's ‘dementia statements’, which they have coproductively developed with 100's of people with experience of dementia or involved in dementia work. The dementia statements were inspired by the UN Convention on the Rights of Persons with Disabilities
(a UN convention focused on the rights of people with a disability – a little known, yet powerful Convention which the UK signed up to in 2006 and which we will be exploring more in later posts).
The dementia statements focus on the ‘rights’
of persons with dementia. The statements are:
1. We have the right to be recognised as who we are, to make choices about our lives including taking risks, and to contribute to society. Our diagnosis should not define us, nor should we be ashamed of it.
2. We have the right to continue with day to day and family life, without discrimination or unfair cost, to be accepted and included in our communities and not live in isolation or loneliness.
3. We have the right to an early and accurate diagnosis, and to receive evidence-based, appropriate, compassionate and properly funded care and treatment, from trained people who understand us and how dementia affects us. This must meet our needs, wherever we live.
4. We have the right to be respected, and recognised as partners in care, provided with education, support, services, and training which enables us to plan and make decisions about the future.
5. We have the right to know about and decide if we want to be involved in research that looks at cause, cure and care for dementia and be supported to take part.
What do you think?
Some startling facts from Jeremy – a third of people with dementia die from a disease rather than dementia. Suggesting that some people with dementia are not being given the treatment they need or not being diagnosed.
The Alzheimer’s Society are doing some fantastic things including the biggest ever population survey of people living with dementia, about their lived experiences. One of the biggest outcomes of this is their use of technology. But Jeremy cautioned that this should not just be about using technology to save money in care. He felt that new technology should mean something to people and not just be a replacement for human contact or conversation.
They are also working with the National Trust
to see how they can make their spaces more accessible to people living with dementia (hurrah!).
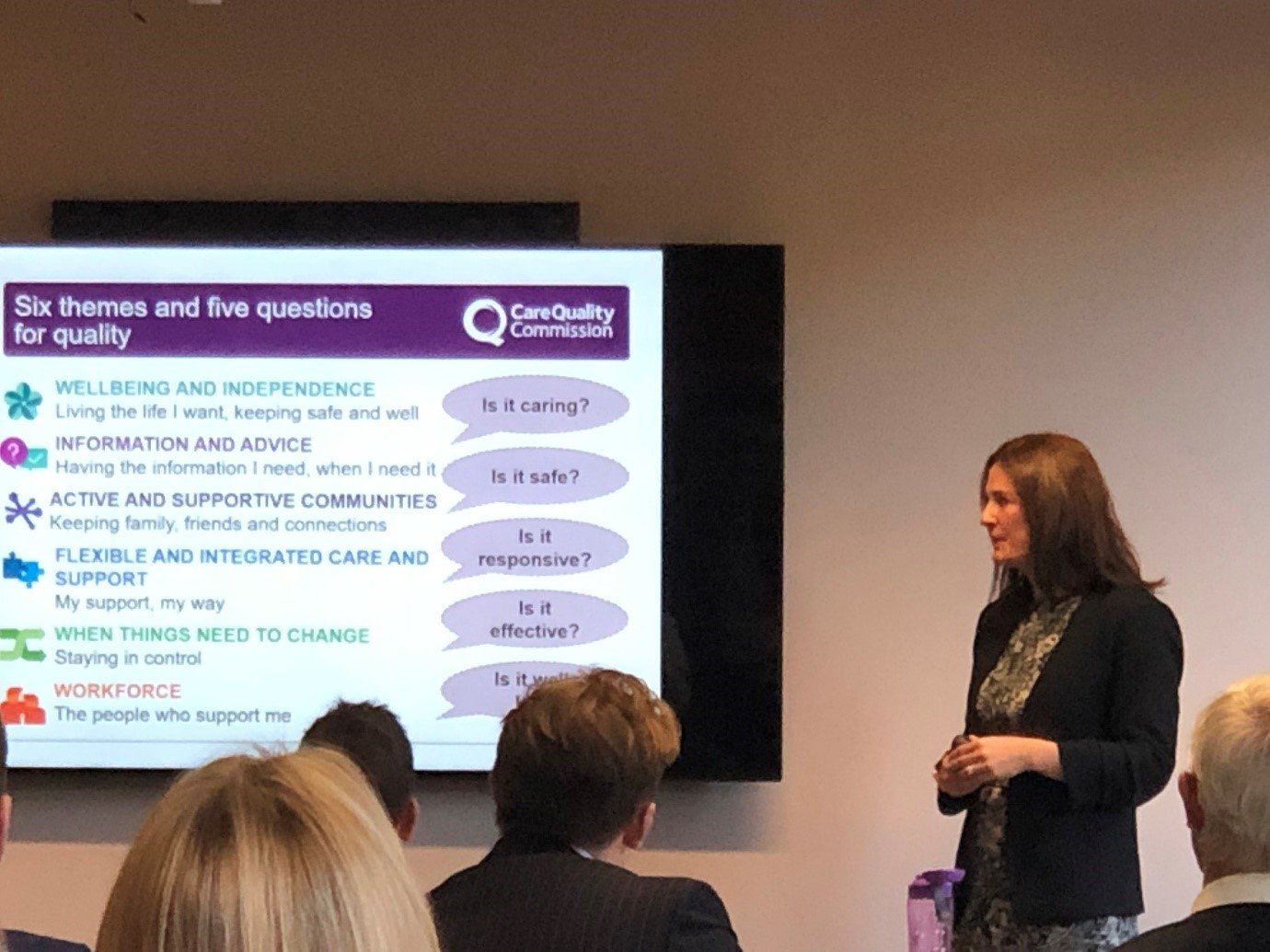
Kate Terroni
The other headline speaker was the newly appointed Chief Inspector of Adult Social Care Kate Terroni
from the Care Quality Commission.
Taking over from Andrea Sutcliffe, she admitted she had big shoes to fill, but if her talk was anything to go by, she will be a key promoter of coproduction and was incredibly open to listening and taking on the views of the people in the room.
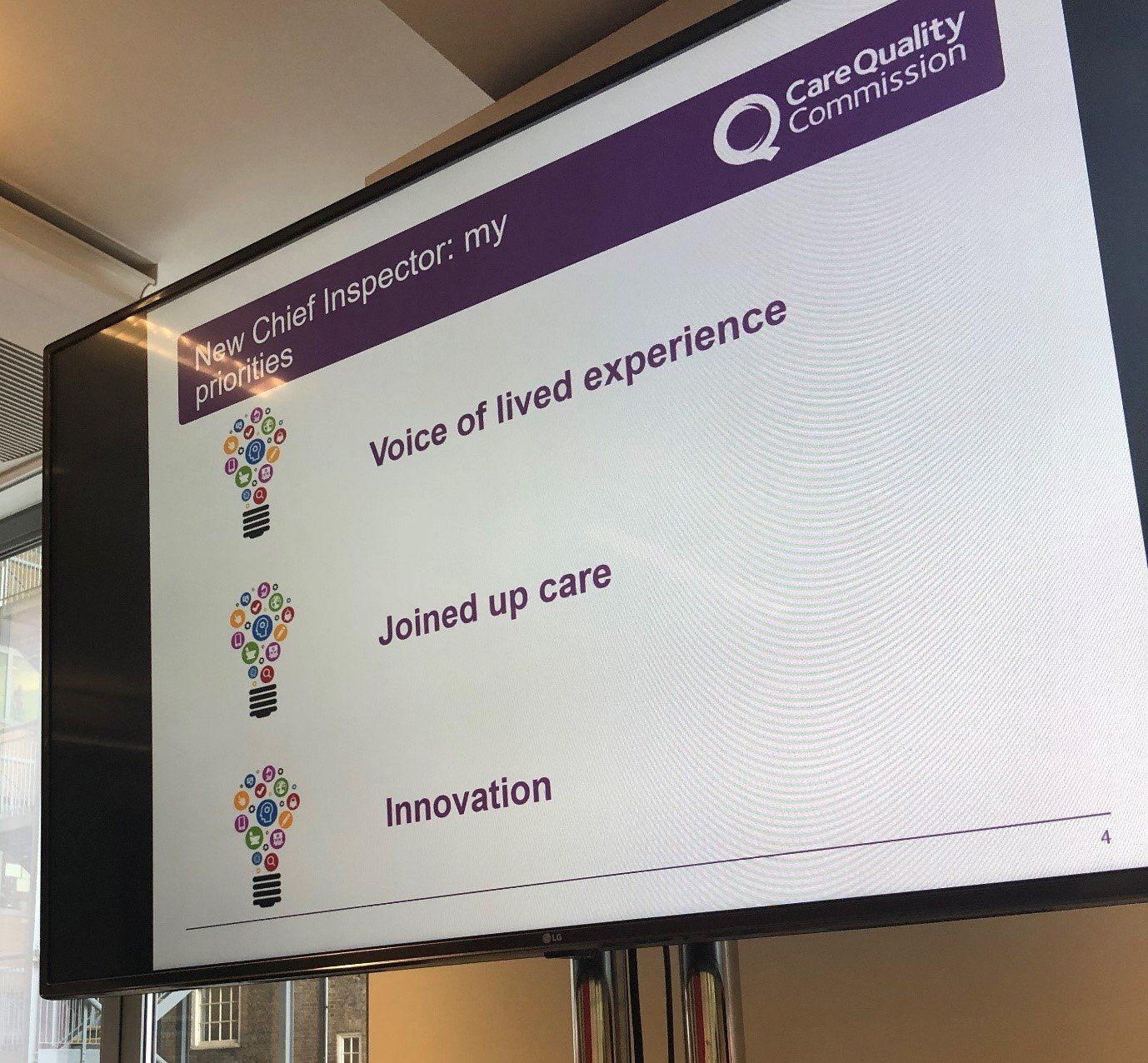
Kate’s focus
Kate discussed her 3 priorities:
1. The voice of lived experience
– we represented people’s voices in care plans, has it been heard and is their lived experience obvious?
2. Joined up care
– to what extent are services working together
3. Innovation
– services should be embarking on innovation that makes a difference to people’s lives.
She highlighted something she heard from Clenton Farquharson
at TLAP:
"good care is about having a life not just a service"
Also, Kate felt that there was a priority to embed coproduction in everything we do as care services and for the CQC as an inspector of services.
Inspections
On inspections, Kate explained that they are making them more concise and shorter.
On new releases from CQC – watch out for a new and frank report on sexual safety in care homes, due for release around November. She warned that it will be quite hard hitting, but Coproduce Care feels these are conversations that need to happen – just because someone is older doesn’t mean they don’t or shouldn’t have sexual relationships!
Medication Errors
Kate pointed out that there are around 237 million medication errors every year. CQC have released a publication on medicine in health and social care. Check it out here.
She also reminded us of the ‘smiling matters’
campaign. You can access their publication on dental care here.
Finally, put 15th October in your diaries as this is when the CQC’s annual ‘State of Care’ will be published. Sign up here
to be notified when the publication of this report goes live. It is important because it is a fantastic summary by the CQC of research and data by them on how the sector is doing. We would encourage you to sign up and we can have a twitter chat about it when it is released!
Join us
We will be relying on a small but dedicated team and volunteers.
So, if you would like to be involved, please get in touch at hi@coproducecare.com
and help us open up the care debate, properly democratise care and please do join and share Coproduce Care:
Spread the word and uncover the hidden opportunities for people-led coproduced care
Recent Posts

We are pleased to provide an update our involvement in new projects currently being undertaken by Coproduce Care (CIC) in collaboration with Care and Support West. We will be contributing to local initiatives in Social Care Workforce Redesign, and we are excited to share the project with you. This project is running from June 2023 to June 2024. We will be working on three areas for the next 10 months all in the BNSSG region which are as follows: 1: Investigation of the Trusted Assessor Approach in Health and Social Care Systems In this project, we are investigating the Trusted Assessor Approach in health and social care systems. The objective is to demonstrate the value of Trusted Assessors in streamlining care needs assessment, while also addressing data protection and consent concerns. Case studies will be created from local regions that have implemented this approach, to provide insights into the benefits of Trusted Assessors of reducing delays in accessing required care. 2: BNSSG Opportunities for Levy Sharing and Increasing Apprenticeships in Social Care This project aims to identify opportunities for levy sharing in social care and increase the use of apprenticeships. The project will engage social care providers, training organizations, authorities, and other stakeholders to develop strategies, guidelines, and an implementation plan for utilizing the levy effectively and increasing the use of apprenticeships. 3: Integrated Health and Social Care: Enhancing Collaboration, Improving Quality, Shaping Models of Care, and the Future Social Care Workforce In this project, we are evidencing the enhanced collaboration between social care providers, health services, and local authorities. By mapping existing interfaces and collaborations, we seek to identify opportunities for cross-system benefits and improved outcomes, creating recommendations for integration for BNSSG. Our research will provide valuable insights to integration and collaboration between social care and health. At Coproduce Care (CIC), we believe that collaboration and innovation are vital for transforming social care. Through these projects, we aim to contribute to a more efficient and compassionate system. We extend our gratitude to all stakeholders, providers, commissioners, and policymakers for their invaluable support. Thank you for your continued interest in our endeavours. We will keep you updated as the projects progresses! In the meantime, if you are doing any work in any of these key areas, please get in touch with us using the below form. Thank you!

Dear Thérèse Coffey, We wish you the best of luck on your appointment as Secretary of State for Health and Social Care. Coproduce Care (CIC) is a non-profit organisation set up to democratise the social care debate. We support the voices of those working and involved in social care to influence wider decision making in the sector. Through our continued work in this area, we are writing to address some of the urgent needs of our social care workforce. We welcome your plans to set out ‘ Our plans for patients ’ to ensure our population have easier access to NHS and social care services through winter, putting the needs of patients as priority. To ensure we prioritise the health and wellbeing of our populations, and deliver the best, high-quality care possible, we need to ensure we prioritise the needs of our workforce who are at the front of delivering health and social care . To ensure both the health and wellbeing of our population and our social care workforce, we recommend the following: 1. Improving pay for social care workers, in real terms The Kings Fund published a report which compared the pay of social care workers to ten of the largest supermarkets. It found that nine out of ten supermarkets paid more than most social care roles. An example used is that if care worker left their role for a supermarket position at Tesco, they would see a 6.3% pay increase instantly. We have conducted many surveys, webinars, and connected with our audience on what is crucial to improving care workers working conditions and we have found that increasing pay is consistently the most crucial factor in reflecting the value of the work and high stress and responsibilities of the role . With the current cost of living crisis, this need for increasing pay is only getting more urgent. The sector currently has 100,000 vacancies , with extremely high levels of staff shortages. This affects the capacity to deliver services and the quality of care provided . Providers are struggling to recruit staff as they are competing with supermarkets and hospitality, sectors of which offer less stress and responsibility and more pay. We believe care workers are an invaluable part of our society and therefore should be paid accordingly. We recommend: · Introduce national pay scales that ensure care workers meet a real national living wage as a minimum . This will recognise the full contribution of social care workers make to the health of our population, and that their contribution is a real investment into our population. By increasing pay, we further increase recruitment and retention in the sector, and improve the perception of social care being a highly valuable and promising career choice. · Facilitate efforts to develop appropriate distribution of funds. Ensuring the integration and professionalisation of care is fully realised will allow better distribution of funds resulting in higher wages which better reflects the level of skill, qualifications, responsibilities and selflessness required to work within this sector. 2. Professionalising the care system Health and social care should be professionalised to encourage staff retention, career progression and further skill development. Professionalising care work would ensure that those working in the sector are valued and are provided with the necessary tools to provide high quality care. Currently, there is no accredited qualification for social care workers, without a standardised training process. We hosted a live stream with Gillian Keegan , who mentioned the government’s intention to create a voluntary digital care workforce hub, as well as a skill passport for all Health & Social Care workers. This is understood to allow easier identification of the workforce, including the possibility to share resources and opportunities to encourage the workforce to up-skill and develop. The skills passport would help keep track of the skills care workers have demonstrated over time, meaning career progression would be easier to identify . Whilst individual action is very important, to improve the quality of care, we urge for a standardised career and training development program for all care staff that results in an accredited qualification . We recommend: · Adequate pay to restore and recognise social care work as a valued profession . Extensive skills are involved in care work, and if standardised training and qualifications are implemented, security of applicable income is appropriate to these expectations. By increasing pay, care work has higher professional footing as a recognised career and role. · Ensuring the integration of social care is fully realised . The high fragmentation of the care sector and its lack of integration with NHS services makes it challenging to implement standardised training . The governments white paper ‘ Health and social care integration: joining up care for people, places and population ’ seeks the ambition to join up social care services. We welcome this white paper and its integration policy to achieve higher quality of care and better health outcomes. This ambition requires effort and commitment to the integration at all levels, and we hope that as health secretary, fully putting this policy into practice and reaching its scope, goals, and purpose is your focus in your new role. · Implementing standardised training, improved learning outcomes for workers, including IT, literacy, and numeracy training are addressed with sensitivity and with the voices of the workers at heart . Implementing standardised training would ensure a level of professionalism across the sector, however, must go in line with the security of increased income and security of hours of work. We must protect the wellbeing of our workforce, of which is already experiencing burn-out and exhaustion from the high pressures the sector is facing. We cannot have higher expectations of our workers undertaking standardised training without adequate pay . We hope you agree with our recommendations and seek to ensure we continue to improve the working conditions for our social care workforce. We hope that within your post as the new Health and Social Care Secretary, you prioritise the voices of those most impacted by decision making regarding the sector. Thank you for taking the time to read this letter, CoProduce Care Written by: Gabriella Neal