Health+Care Conference 2019 - Day 2 Summary
Sophie Chester-Glyn • 28 June 2019
Starting with my summary
I’d initially planned on whizzing around the theatres like yesterday. However, with Matt Hancock’s Special Advisor
talking about his work, Cambridge and Peterborough STP
discussing parity of esteem, NHSX
pre-launch keynote address and CQC’s Ian Trenholm’s
thoughts on the regulatory system, I was firmly planted in the Healthcare’s Keynote Theatre all day.
Reflections from Richard Sloggett – Matt Hancock’s Special Advisor
Richard explained that his job is unsurprisingly fast-paced, with his first experiences involving swatting up on acronyms to translate NHS policies it into public friendly messages. Possibly the most revealing (and random) part of Richard’s revelations was the ‘red box’ which, from what I could make out, was Matt Hancock’s in-tray. Anything that goes in it will be on his radar and must be addressed. Richard spent the majority of his day trying to clear the red box. Sensing the audience’s confusion, chairman Professor Paul Corrigan
explained that this was part of how the constitution worked – if the Minister doesn’t see something and agree it, it isn’t happening. Makes sense.
Something to look out for is the prevention green paper
due out in July. Amongst other things this aims to cover what the government will provide and what they expect citizens to do in terms of preventing their own health deterioration. For Richard, the real point on prevention was population health management and that Integrated Care Services (ICSs) should be well place to deliver this.
He reminded us that next week on 1st July Primary Care Networks
(PCNs) go live. The funding that is being allocated to PCNs should be filtered out to its partners – I think we all have a role in ensuring that this happens, especially since they will be rewarded financially if, for example, their activities reduce A&E admissions. Question is how will this be monitored?
Richard ended his talk with the observation that currently, as represented by the exhibitors at the conference, technology in care is 'explosive'.
Parity of esteem in mental health
The question for this panel was 'Parity of esteem in mental health - is this the time to make it really happen?'. The panel included Lorna Evans
from Cambridgeshire and Peterborough NHS Foundation Trust, Emma Tiffin
from Cambridgeshire and Peterborough STP and Sarah Hughes, Chief Executive of Centre for Mental Health. Lorna gave a heartwarming explanation of her own experiences of mental struggles following personal strategies – a strong user voice, maybe because user voices were not well represented at the conference, an improvement for next year maybe? Her insight into how Cambridgeshire promoted its Community Based Crisis Support helpline through 111 option 2, represented a key point of access and clear attempt to create practical parity.
Other important attempts at parity expressed by this panel include:
- Focusing on peer support
- Equally well
A great point prompted from an audience member's observation of the New Zealand’s model, came from Sarah. She felt that the political leadership in New Zealand was itself progressive and the UK was far behind that. Therefore, without a PM that is as progressive as theirs, we all need to become activists in our area and push for the change we want to see.
Do we need legislative change to make the NHS long term plan happen?
Paul Maubach (presenting) and Niall Dickson
The short answer from Paul Maubach, CEO of Dudley CCO, was yes! His justification was that it would align incentives and practices and integrate providers. He argued that our legislation currently favours competition not collaboration and creates separation between the commissioner and provider. The change should instead privilege collaboration between the two. The Health and Social Care Act 2012 doesn’t, according the Paul, facilitate this. In fact I feel that this video
by the Kings Fund from 2013 is still relevant in representing the complex quagmire of services, actors and initiatives that have been created:
Niall Dickson, from NHS Confederating listed his take on the challenge, including:
- A need for a ‘bet value test’ that is less subjective
- Greater flexibility locally, arguing that the NHS should produce on quality not price
- He recognised that there is a fear in the social community sphere of there being an ‘Acute Takeover’ and that they will be subsumed into larger NHS provision
Both Niall and Paul agreed that the 2012 Act should ideally be repealed. However, acknowledge the political unpopularity of this idea.
NHSX pre-lauch keynote by its CEO, Matthew Gould
Large queues formed 15 minutes before this talk, representing a general buzz around NHSX. In fact after the talk I personally wasn’t too much clearer about what it would actually look like, but got the sense that neither did anyone else. The mission, however, was clear and very interesting. For a high-level intro, listen to this 5 min video from Matt Hancock
Matthew’s Gould's keynote address included these key messages:
NHSX is a new single decision-making team bringing everything tech related together to give patients and staff the technology they need.
What’s different? Not imposing top down decision on Trusts and CCG’s but instead letting professionals work together for local solutions. His aim was to ‘keep the centre thin’ and to create platforms from which others can develop on, but keep some things central such as screening and booking systems.
It will have 5 missions which include:
- Reduced burdens on staff so they can focus on patients
- Giving citizens the tools to access information and services directly
- Ensuring clinical information is safe and digitally accessed
- Improving patient safety across the NHS and
- Increasing productivity across NHS
A great question from the audience was, how would we know they are effective in say 2 years time? Matthew thought for a moment then suggested we judge NHSX against these 5 missions and at the very least on the fact of whether NHSX has made any impact at all. He argued that it really should have by then.
A few people also pointed out the Long Term Plan’s ambition to go paperfree by 2020. From the examples of poor systems in his talk, it was clear that this isn’t going to happen by then, but he was clear that it was still in their plans.
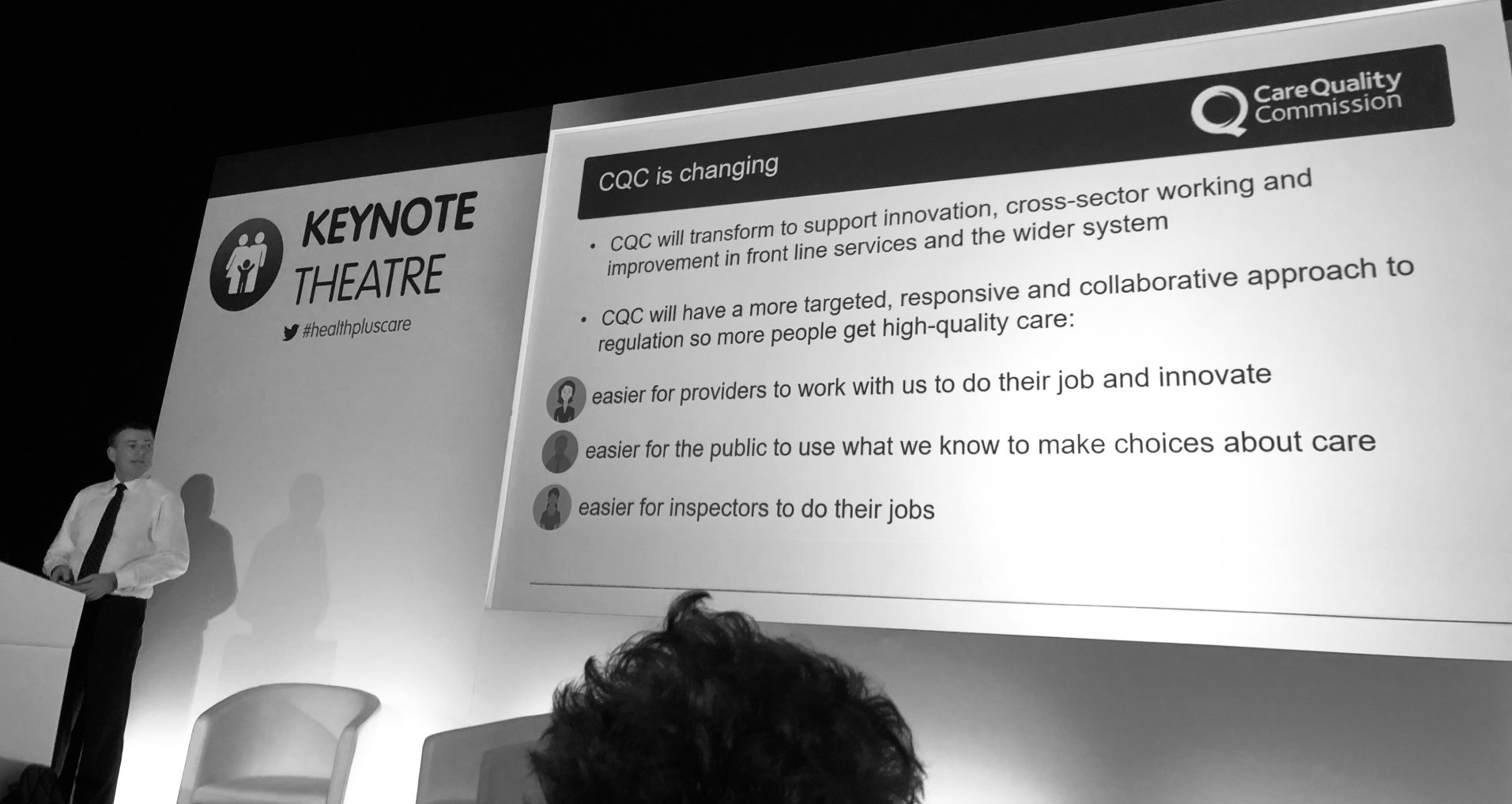
Ian Trenholm - CQC's Chief Executive on the future of inspection
Another key leader in health and care, Ian Treholme, led the penultimate talk of the day. He remarked that CQC is still going on a journey but had a built up a reputation as a regulator with a methodology he felt worked. He showed frustration about the fact that CQC collects a lot of positive stories which are unrepresented by the media. Made me think, maybe this is where as a sector we can pick up on this and start sharing positive stories on platforms such as social media?
Ian mentioned that following the revelations at Wholton Hall by Panorama, the CQC went through and is still going through a process of reflection, asking: how was this able to happen? What could have been done differently to detect that the abuse might have occurred?
They are going to investigate internally. I felt this critical reflective type practice was refreshingly honest. He explained that the future may include a digital solution to get poor practice evidence to them quicker from those using services and staff.
Ensuring safe technology by working with NHSX was a key passion.
In terms of personalised care, he was unequivocal that CQC will be inspecting services from the standpoint o effectiveness from a patient perspective. They will be expecting leadership to show how they are working collaboratively to enable this. This will be a key part of ‘Well-led’. I got the impression that without evidence of this collaborative working for better care, the top CQC ratings will start to become out of reach.
He mentioned that CQC are starting to review their regulatory process. They will be moving away from periodic reviews, whereby good or outstanding services are visited less often than others, and moving towards risk-based inspections. When I asked him to clarify this, it appears that the plans are very young and providers will be consulted, so keep an eye out for this consultation and please get involved.
Ian Treholme
Questions from the audience for Ian
One audience member asked Ian about his views on families putting cameras in people’s bedrooms. Ian pointed out that pre-Wholton Hall he probably would have been more certain on an answer to this. Post-Wholton Hall, the jury was out and he understood the arguments for and against in terms of revealing poor practice which CQC might be unable to detect verses respecting a person's dignity and human rights.
My last question to him and I think to every really, was/is:
considering the push towards social prescribing, pushed through by PCNs, we will most likely see a lot of services traditionally provided by regulated providers, slowly and informally migrating to community groups and organisations. Should social prescribing be regulated in some way?
Understandably, seeing that PCNs are so new, there was no firm answer to this, but maybe a point to consider.
The last session from the Keynote Theatre
The last session was possibly the most lively one, with a full panel including Caroline Abrahams from Age UK, Lord Victor Adebowale
from Turning Point, Clare Gerada frm NHS Assembly
and Sir Robert Francis QC, Chair of Healthwatch Engand.
The panel was clear on the need to engage and consult with patients on strategic decision-making, but were not as clear on the role of enforcing coproduction (which I’m fan of and asked about). Other points included:
- Sir Francis promoting what I would term a dialectical approach with citizens to strategic decision-making
- Lord Victor Adebowale was concerned about ‘racist algorithms’ in technology, staff shortages and discrimination. Interestingly, he will be editing the BMJ’s next edition with a focus on discrimination – will be keeping and eye out on this.
- A great quote from Lord Adebowale was that ‘culture eats structure for breakfast’ and without a culture change, we can create all the STPs etc but will still operate top down.
Finally, from me...
Finally, someone from the audience was from Think Local Act Personal (TLAP)
and put in a plug to their Making It Real initiative, which they had made every effort to promote, but were still not seeing enough take up. This is a great shame. TLAP have effectively coproduced quality marks for health and social care. We (Manor Community), were early adopters and used Making It Real in a pilot
and continue to do so.
Maybe people just do not understand what coproduction is!? The co-opting and misunderstanding of coproduction is a huge bugbear for me. I would urge people to check out and share TLAPs coproduction ladder and ask their leadership which step they operate on on the coproduction ladder?!
The TLAP question mirrors an important issue across the two days – the tools are there, it’s just making sure they get used and known by the right people and embedded into their culture.
Other nuggets from the rest of our team at the conference:
- Leicestershire County Council’s ‘housing support coordinator’ link role as part of a centralised program bringing different health and well-being support together to make more holistic preventative care plans to help move people out of hospital
- The Richmond Group of charities and their social prescribing collaboration across care, health and VSCE across Somerset.
- The King’s Fund’s recently published report on Wigan Council. Wigan Council ran a coproduced collaborative community development scheme that has been specifically linked to health benefits and mental health
- Clare from Care Forum Tech Transformation pointed out that we shouldn’t use tech for its own sake but keep in focus what difference does it makes for helping enhance relationships and that the person is at the centre of change.
That’s it from us! Hope it’s helpful, feel free to share if it is.
Sophie
and the team @coproducecare
Recent Posts

We are pleased to provide an update our involvement in new projects currently being undertaken by Coproduce Care (CIC) in collaboration with Care and Support West. We will be contributing to local initiatives in Social Care Workforce Redesign, and we are excited to share the project with you. This project is running from June 2023 to June 2024. We will be working on three areas for the next 10 months all in the BNSSG region which are as follows: 1: Investigation of the Trusted Assessor Approach in Health and Social Care Systems In this project, we are investigating the Trusted Assessor Approach in health and social care systems. The objective is to demonstrate the value of Trusted Assessors in streamlining care needs assessment, while also addressing data protection and consent concerns. Case studies will be created from local regions that have implemented this approach, to provide insights into the benefits of Trusted Assessors of reducing delays in accessing required care. 2: BNSSG Opportunities for Levy Sharing and Increasing Apprenticeships in Social Care This project aims to identify opportunities for levy sharing in social care and increase the use of apprenticeships. The project will engage social care providers, training organizations, authorities, and other stakeholders to develop strategies, guidelines, and an implementation plan for utilizing the levy effectively and increasing the use of apprenticeships. 3: Integrated Health and Social Care: Enhancing Collaboration, Improving Quality, Shaping Models of Care, and the Future Social Care Workforce In this project, we are evidencing the enhanced collaboration between social care providers, health services, and local authorities. By mapping existing interfaces and collaborations, we seek to identify opportunities for cross-system benefits and improved outcomes, creating recommendations for integration for BNSSG. Our research will provide valuable insights to integration and collaboration between social care and health. At Coproduce Care (CIC), we believe that collaboration and innovation are vital for transforming social care. Through these projects, we aim to contribute to a more efficient and compassionate system. We extend our gratitude to all stakeholders, providers, commissioners, and policymakers for their invaluable support. Thank you for your continued interest in our endeavours. We will keep you updated as the projects progresses! In the meantime, if you are doing any work in any of these key areas, please get in touch with us using the below form. Thank you!

Dear Thérèse Coffey, We wish you the best of luck on your appointment as Secretary of State for Health and Social Care. Coproduce Care (CIC) is a non-profit organisation set up to democratise the social care debate. We support the voices of those working and involved in social care to influence wider decision making in the sector. Through our continued work in this area, we are writing to address some of the urgent needs of our social care workforce. We welcome your plans to set out ‘ Our plans for patients ’ to ensure our population have easier access to NHS and social care services through winter, putting the needs of patients as priority. To ensure we prioritise the health and wellbeing of our populations, and deliver the best, high-quality care possible, we need to ensure we prioritise the needs of our workforce who are at the front of delivering health and social care . To ensure both the health and wellbeing of our population and our social care workforce, we recommend the following: 1. Improving pay for social care workers, in real terms The Kings Fund published a report which compared the pay of social care workers to ten of the largest supermarkets. It found that nine out of ten supermarkets paid more than most social care roles. An example used is that if care worker left their role for a supermarket position at Tesco, they would see a 6.3% pay increase instantly. We have conducted many surveys, webinars, and connected with our audience on what is crucial to improving care workers working conditions and we have found that increasing pay is consistently the most crucial factor in reflecting the value of the work and high stress and responsibilities of the role . With the current cost of living crisis, this need for increasing pay is only getting more urgent. The sector currently has 100,000 vacancies , with extremely high levels of staff shortages. This affects the capacity to deliver services and the quality of care provided . Providers are struggling to recruit staff as they are competing with supermarkets and hospitality, sectors of which offer less stress and responsibility and more pay. We believe care workers are an invaluable part of our society and therefore should be paid accordingly. We recommend: · Introduce national pay scales that ensure care workers meet a real national living wage as a minimum . This will recognise the full contribution of social care workers make to the health of our population, and that their contribution is a real investment into our population. By increasing pay, we further increase recruitment and retention in the sector, and improve the perception of social care being a highly valuable and promising career choice. · Facilitate efforts to develop appropriate distribution of funds. Ensuring the integration and professionalisation of care is fully realised will allow better distribution of funds resulting in higher wages which better reflects the level of skill, qualifications, responsibilities and selflessness required to work within this sector. 2. Professionalising the care system Health and social care should be professionalised to encourage staff retention, career progression and further skill development. Professionalising care work would ensure that those working in the sector are valued and are provided with the necessary tools to provide high quality care. Currently, there is no accredited qualification for social care workers, without a standardised training process. We hosted a live stream with Gillian Keegan , who mentioned the government’s intention to create a voluntary digital care workforce hub, as well as a skill passport for all Health & Social Care workers. This is understood to allow easier identification of the workforce, including the possibility to share resources and opportunities to encourage the workforce to up-skill and develop. The skills passport would help keep track of the skills care workers have demonstrated over time, meaning career progression would be easier to identify . Whilst individual action is very important, to improve the quality of care, we urge for a standardised career and training development program for all care staff that results in an accredited qualification . We recommend: · Adequate pay to restore and recognise social care work as a valued profession . Extensive skills are involved in care work, and if standardised training and qualifications are implemented, security of applicable income is appropriate to these expectations. By increasing pay, care work has higher professional footing as a recognised career and role. · Ensuring the integration of social care is fully realised . The high fragmentation of the care sector and its lack of integration with NHS services makes it challenging to implement standardised training . The governments white paper ‘ Health and social care integration: joining up care for people, places and population ’ seeks the ambition to join up social care services. We welcome this white paper and its integration policy to achieve higher quality of care and better health outcomes. This ambition requires effort and commitment to the integration at all levels, and we hope that as health secretary, fully putting this policy into practice and reaching its scope, goals, and purpose is your focus in your new role. · Implementing standardised training, improved learning outcomes for workers, including IT, literacy, and numeracy training are addressed with sensitivity and with the voices of the workers at heart . Implementing standardised training would ensure a level of professionalism across the sector, however, must go in line with the security of increased income and security of hours of work. We must protect the wellbeing of our workforce, of which is already experiencing burn-out and exhaustion from the high pressures the sector is facing. We cannot have higher expectations of our workers undertaking standardised training without adequate pay . We hope you agree with our recommendations and seek to ensure we continue to improve the working conditions for our social care workforce. We hope that within your post as the new Health and Social Care Secretary, you prioritise the voices of those most impacted by decision making regarding the sector. Thank you for taking the time to read this letter, CoProduce Care Written by: Gabriella Neal