The Bi-annual conference for NHS Employee Wellbeing
Sophie Chester-Glyn • 7 October 2019
In September we attended the Westminster Insight
bi-annual conference for NHS Employee
Well-being to hear from trailblazing front line professionals including, NHS leaders, the Royal College of Nursing, Skills for Health and Health Education England on how to improve mental health and well-being provisions for your employees. In our quest to open up the care debate, read our summary of the conference here.
The event was chaired by Sir John Burn
(Chair of Newcastle Hospitals NHS Foundation Trust and non-executive director of NHS England). The first talk, by Simon Gregory, reminded us of the Tea and Empathy Facebook page
which provides informal peer support for NHS staff and describes itself as a national, informal, peer-to-peer support network aiming to foster a compassionate and supportive atmosphere throughout the NHS. He also highlighted that whilst people in the NHS often focus on supporting others, it is often their own staffs’ personal comfort which suffers as a result with around 38% of staff missing a meal break during their working week and mainly clerical staff suffering in terms of well-being.
In line with a key recommendation made in the Health Education England’s (HEE) NHS Staff and Learners’ Mental Wellbeing Commission report, there has been increasing pressure
to introduce well-being guardians into the NHS for NHS staff. A well-being guardian would be a dedicated person, trained to recognise and support staff when they are experiencing difficulties. NHS Improvement and HEE are looking at taking this forward with a group led by Dr. Paul Litchfield.
Professor Pauline Walsh, Pro Vice Chancellor (Health and Wellbeing) and Executive Dean, Faculty of Medicine and Health Sciences, Keele Univeristy and, Chair of Education Forum Royal College of Nursing.
Pauline focused her talk on the well-being of medical students. She highlighted that students are ill equipped for the clinical placements and heavy workload which face them after medical school. She also pointed to the social isolation in education.
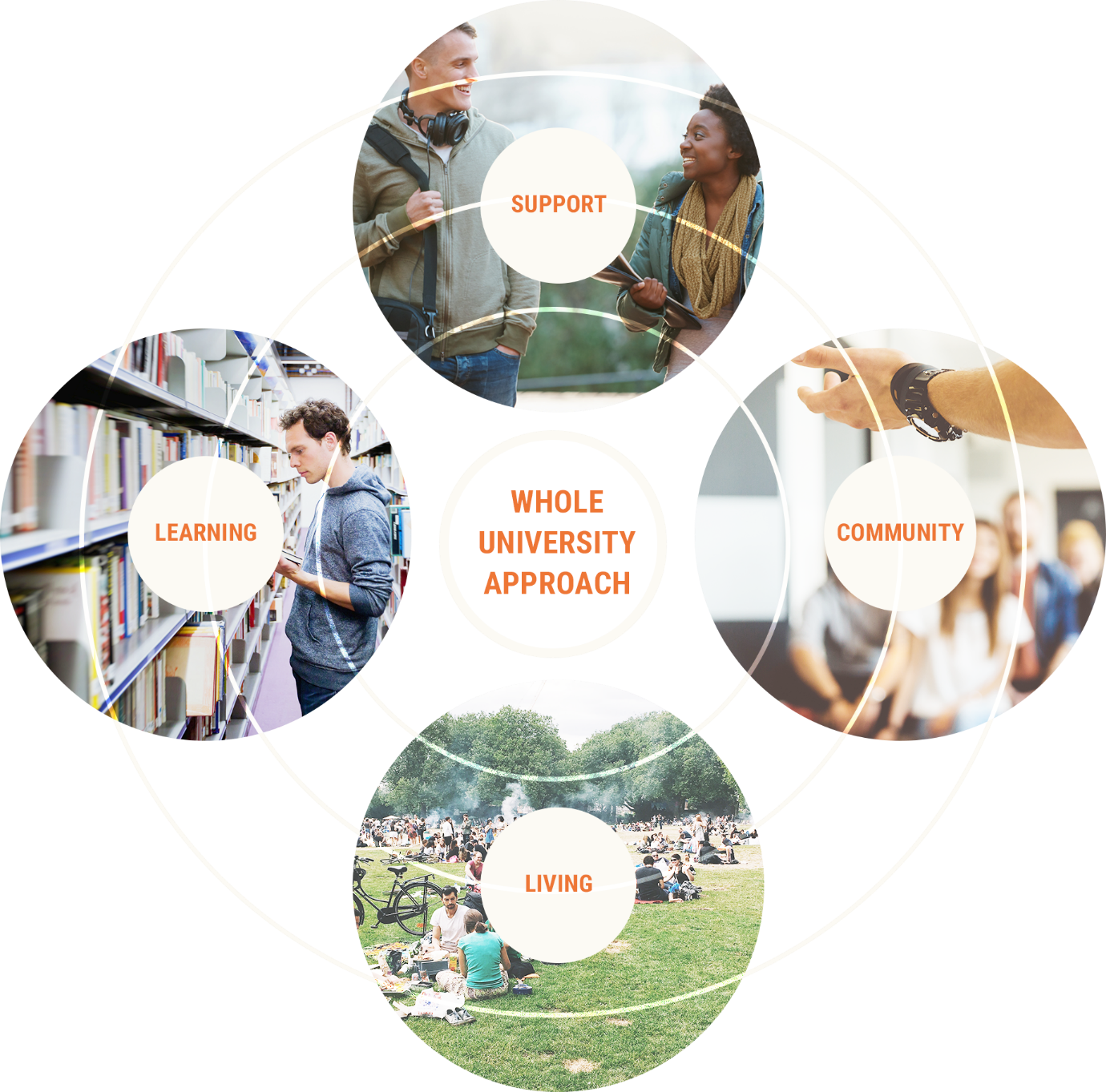
In terms of student health, the Pauline pointed out that the Universities UK (UUK) Step Change Programme
led by professor Steven West
at the University of the West of England (UWE) considers mental health in terms of a whole university approach such as the individual support provided to students and community support. She also suggests that institutions should:
- See students as individuals not just data.
- Realise that managing transitions from university to the NHS are vital and that this is best achieved through a partnership approach with students and university and clinician placements.
- Recognise the need to accept difference and diversity.
Pauline also elaborated on what they are doing at Keele University which include to support health student’s mental health. This included:
- NHS staff and learners mental wellbeing support
- HEE RePAIR Programme. RePAIR stands for Reducing Attrition and Improving Retention project. It has enabled Health Education England (HEE) to gain an in-depth understanding of the factors impacting on healthcare student attrition and the retention of the newly qualified workforce in the early stages of their careers.
- Supporting UUK Stepchange
Lynn Demeda, Director of Workforce Programmes
The morning session concluded with an interesting case study talk from Lynn Demeda, Director of Workforce Programmes, Guy’s and St Thomas NHS Foundation Trust. Lynn was passionate about concentrating on changing workers' experiences, spurred on by the fact that only 55% of staff surveyed were happy with the flexible working arrangements available, which she felt was not good enough.
Lynn surmised that, whilst we care for our patients, we need to support our staff in the same way and that there needs to be person centredness in this approach as ‘one size does not fit all’. For her, the biggest thing that helped improve organisational culture in NHS, is a human conversation and feeling comfortable about talking.
Some of the things they’re doing in her hospital includes improvements to people practices such as:
- Focusing on values and behaviours.
- Human conversations rather than formal processes, senior managers being given time to have coffee with their staff
- There should be a deeper focus on staff data/feedback/survey and complaints.
- People coming together to solve issues, such as talking about bullying and speaking truth to power and making senior leaders see things from a different perspective (this sounds a lot like coproduction to us!).
A recurring theme was allowing people to take a break, supporting work life balance and her summary was that people working in health should be curious about data and understand what staff think. They should also recognise that small things can be an impact such as overnight food for doctors, review of the ‘good work standards’ and digital well-being initiatives.
The afternoon session started with a panel which included Dr Benedict Eccles
from Skills for Health, Professor Wendy Reid
(Director for Education and Quality Health Education England) and Professor Dinesh Bhugra CBE
(president of the BMA council).
Dr Benedict Eccles from skills for health felt that NHS Employee well-being was an ongoing issue which felt a bit like déjà vu or what he termed to be a ‘festival of words’ whereby the issue of well-being and mental health of staff had been something which, having been identified several decades ago, has yet to be solved, but continues to be discussed.
Professor Wendy Reid mused that the NHS should have a personalised training programme as a right for staff. Whilst not directly linked to well-being, a question from the audience about admission into the profession being strict and contributing to staffing issues prompted Wendy to reveal some potential changes afoot. She pointed out that currently 27% schools do not teach chemistry and there is growing support to open up psychology to the admissions criteria so that it is seen on a par with chemistry, which could have a significant impact to student numbers. At the moment, school leavers need (in the previous GCSE grading) 3 A's and an A* in chemistry. This could all change.
Professor Dinesh spoke of some alarming statistics from an international survey including 12 countries, regarding the mental health and well-being for trainees and qualified medics. It found that 88% of respondents felt that they had suffered burn-out. Other findings included that a lot of the issues were structural, there had been a mechanisation of medicine and that for him, we ought to revisit ‘medicine’s social contract’. He discusses the idea of medicine’s social contract in more detail here.
Comment below in anything you found interesting in this conference summary and as usual feel free to share.
This Facebook widget is no longer supported.
Join us
We will be relying on a small but dedicated team and volunteers.
So, if you would like to be involved, please get in touch at hi@coproducecare.com
and help us open up the care debate, properly democratise care and please do join and share Coproduce Care:
Spread the word and uncover the hidden opportunities for people-led coproduced care
Recent Posts

We are pleased to provide an update our involvement in new projects currently being undertaken by Coproduce Care (CIC) in collaboration with Care and Support West. We will be contributing to local initiatives in Social Care Workforce Redesign, and we are excited to share the project with you. This project is running from June 2023 to June 2024. We will be working on three areas for the next 10 months all in the BNSSG region which are as follows: 1: Investigation of the Trusted Assessor Approach in Health and Social Care Systems In this project, we are investigating the Trusted Assessor Approach in health and social care systems. The objective is to demonstrate the value of Trusted Assessors in streamlining care needs assessment, while also addressing data protection and consent concerns. Case studies will be created from local regions that have implemented this approach, to provide insights into the benefits of Trusted Assessors of reducing delays in accessing required care. 2: BNSSG Opportunities for Levy Sharing and Increasing Apprenticeships in Social Care This project aims to identify opportunities for levy sharing in social care and increase the use of apprenticeships. The project will engage social care providers, training organizations, authorities, and other stakeholders to develop strategies, guidelines, and an implementation plan for utilizing the levy effectively and increasing the use of apprenticeships. 3: Integrated Health and Social Care: Enhancing Collaboration, Improving Quality, Shaping Models of Care, and the Future Social Care Workforce In this project, we are evidencing the enhanced collaboration between social care providers, health services, and local authorities. By mapping existing interfaces and collaborations, we seek to identify opportunities for cross-system benefits and improved outcomes, creating recommendations for integration for BNSSG. Our research will provide valuable insights to integration and collaboration between social care and health. At Coproduce Care (CIC), we believe that collaboration and innovation are vital for transforming social care. Through these projects, we aim to contribute to a more efficient and compassionate system. We extend our gratitude to all stakeholders, providers, commissioners, and policymakers for their invaluable support. Thank you for your continued interest in our endeavours. We will keep you updated as the projects progresses! In the meantime, if you are doing any work in any of these key areas, please get in touch with us using the below form. Thank you!

Dear Thérèse Coffey, We wish you the best of luck on your appointment as Secretary of State for Health and Social Care. Coproduce Care (CIC) is a non-profit organisation set up to democratise the social care debate. We support the voices of those working and involved in social care to influence wider decision making in the sector. Through our continued work in this area, we are writing to address some of the urgent needs of our social care workforce. We welcome your plans to set out ‘ Our plans for patients ’ to ensure our population have easier access to NHS and social care services through winter, putting the needs of patients as priority. To ensure we prioritise the health and wellbeing of our populations, and deliver the best, high-quality care possible, we need to ensure we prioritise the needs of our workforce who are at the front of delivering health and social care . To ensure both the health and wellbeing of our population and our social care workforce, we recommend the following: 1. Improving pay for social care workers, in real terms The Kings Fund published a report which compared the pay of social care workers to ten of the largest supermarkets. It found that nine out of ten supermarkets paid more than most social care roles. An example used is that if care worker left their role for a supermarket position at Tesco, they would see a 6.3% pay increase instantly. We have conducted many surveys, webinars, and connected with our audience on what is crucial to improving care workers working conditions and we have found that increasing pay is consistently the most crucial factor in reflecting the value of the work and high stress and responsibilities of the role . With the current cost of living crisis, this need for increasing pay is only getting more urgent. The sector currently has 100,000 vacancies , with extremely high levels of staff shortages. This affects the capacity to deliver services and the quality of care provided . Providers are struggling to recruit staff as they are competing with supermarkets and hospitality, sectors of which offer less stress and responsibility and more pay. We believe care workers are an invaluable part of our society and therefore should be paid accordingly. We recommend: · Introduce national pay scales that ensure care workers meet a real national living wage as a minimum . This will recognise the full contribution of social care workers make to the health of our population, and that their contribution is a real investment into our population. By increasing pay, we further increase recruitment and retention in the sector, and improve the perception of social care being a highly valuable and promising career choice. · Facilitate efforts to develop appropriate distribution of funds. Ensuring the integration and professionalisation of care is fully realised will allow better distribution of funds resulting in higher wages which better reflects the level of skill, qualifications, responsibilities and selflessness required to work within this sector. 2. Professionalising the care system Health and social care should be professionalised to encourage staff retention, career progression and further skill development. Professionalising care work would ensure that those working in the sector are valued and are provided with the necessary tools to provide high quality care. Currently, there is no accredited qualification for social care workers, without a standardised training process. We hosted a live stream with Gillian Keegan , who mentioned the government’s intention to create a voluntary digital care workforce hub, as well as a skill passport for all Health & Social Care workers. This is understood to allow easier identification of the workforce, including the possibility to share resources and opportunities to encourage the workforce to up-skill and develop. The skills passport would help keep track of the skills care workers have demonstrated over time, meaning career progression would be easier to identify . Whilst individual action is very important, to improve the quality of care, we urge for a standardised career and training development program for all care staff that results in an accredited qualification . We recommend: · Adequate pay to restore and recognise social care work as a valued profession . Extensive skills are involved in care work, and if standardised training and qualifications are implemented, security of applicable income is appropriate to these expectations. By increasing pay, care work has higher professional footing as a recognised career and role. · Ensuring the integration of social care is fully realised . The high fragmentation of the care sector and its lack of integration with NHS services makes it challenging to implement standardised training . The governments white paper ‘ Health and social care integration: joining up care for people, places and population ’ seeks the ambition to join up social care services. We welcome this white paper and its integration policy to achieve higher quality of care and better health outcomes. This ambition requires effort and commitment to the integration at all levels, and we hope that as health secretary, fully putting this policy into practice and reaching its scope, goals, and purpose is your focus in your new role. · Implementing standardised training, improved learning outcomes for workers, including IT, literacy, and numeracy training are addressed with sensitivity and with the voices of the workers at heart . Implementing standardised training would ensure a level of professionalism across the sector, however, must go in line with the security of increased income and security of hours of work. We must protect the wellbeing of our workforce, of which is already experiencing burn-out and exhaustion from the high pressures the sector is facing. We cannot have higher expectations of our workers undertaking standardised training without adequate pay . We hope you agree with our recommendations and seek to ensure we continue to improve the working conditions for our social care workforce. We hope that within your post as the new Health and Social Care Secretary, you prioritise the voices of those most impacted by decision making regarding the sector. Thank you for taking the time to read this letter, CoProduce Care Written by: Gabriella Neal