Event by the King’s Fund: Community is the best Medicine
Sophie Chester-Glyn • 9 October 2019
Making a reality of community-based health
The King’s Fund
is a leading think-tank and independent charity which holds regular health and social care events, shares research and commentary. Whilst the King’s Fund has traditionally focused on health-related topics, it is increasingly shining the light on leadership and community developments in social care. This latest event on community-led care and support is an example of this. We were lucky to attend. See our blog summary below.
After an introductory session, events at The King’s Fund are typically split up into break-out sessions. Whilst we weren’t able to attend all of these, here are our main take-aways.
The plenary session was chaired by The Kings Fund’s David Buck
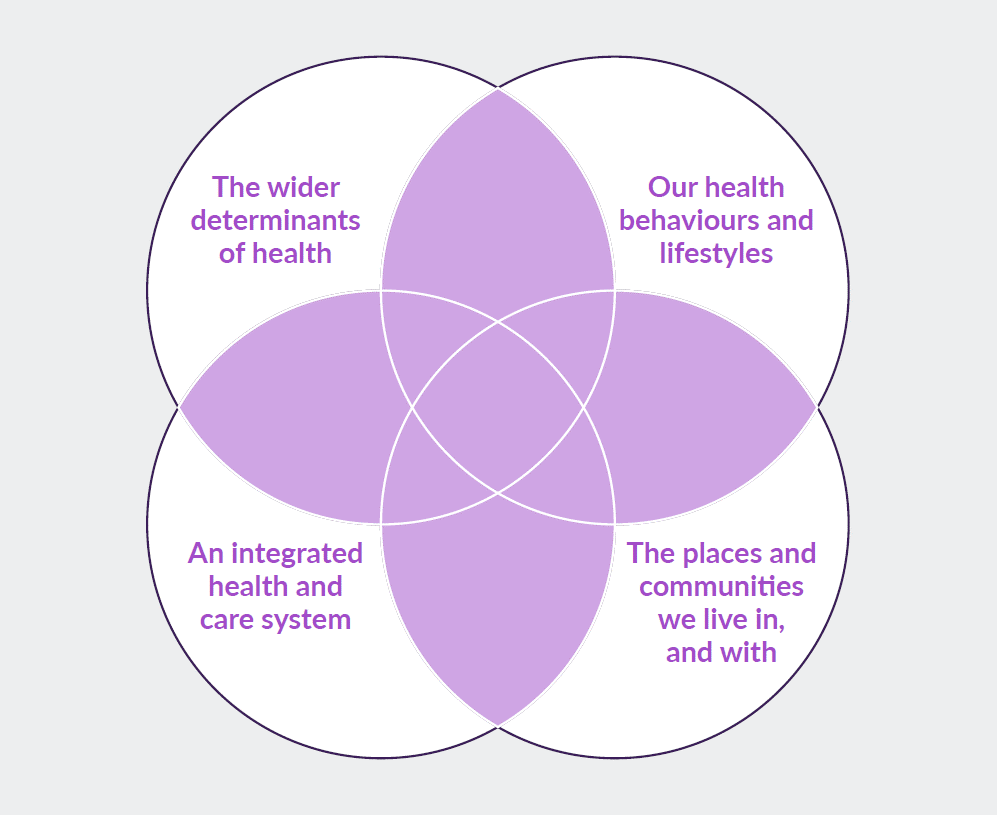
(senior fellow specialising in public health and health inequalities). David pointed out that as a country we are living longer yet are less healthy. Whilst this is nothing new, the concept of population health is possibly a less familiar concept to non-health professionals. David reminded us that population health
is one of the key focuses of The King’s Fund’s work and concerns the intersection (see the purple section below) between health behaviours, systems, the wider determinants of health and communities. Today’s event was focusing on the latter.
Next, Professor Jane South, National Adviser on Communities from Public Health England, started us off with a look back at the reviews considering the benefits of assets within our communities. She reminded us of the literature over recent years, which builds up the academic and policy case for better community-centred approaches to improve health and reduce inequalities, such as:
- The Marmot Review – ‘Fair Society, Healthy Lives’
- Public Health England – ‘From evidence into action: opportunities to protect and improve the nation’s health’
- NHS – ‘Five Year Forward View’
- HM Government – Civil Society Strategy: Building A Future that Works for Everyone.
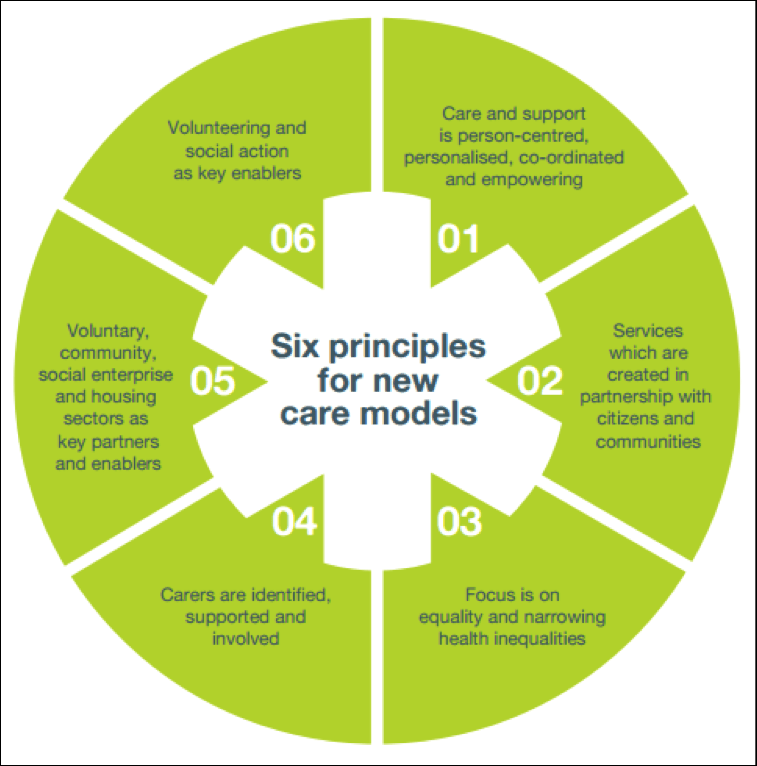
- National Voices – ‘New Model Partnership people and communities’
Her message was to consider how health benefits and services can be delivered ‘with’ rather than simply ‘to’ people.
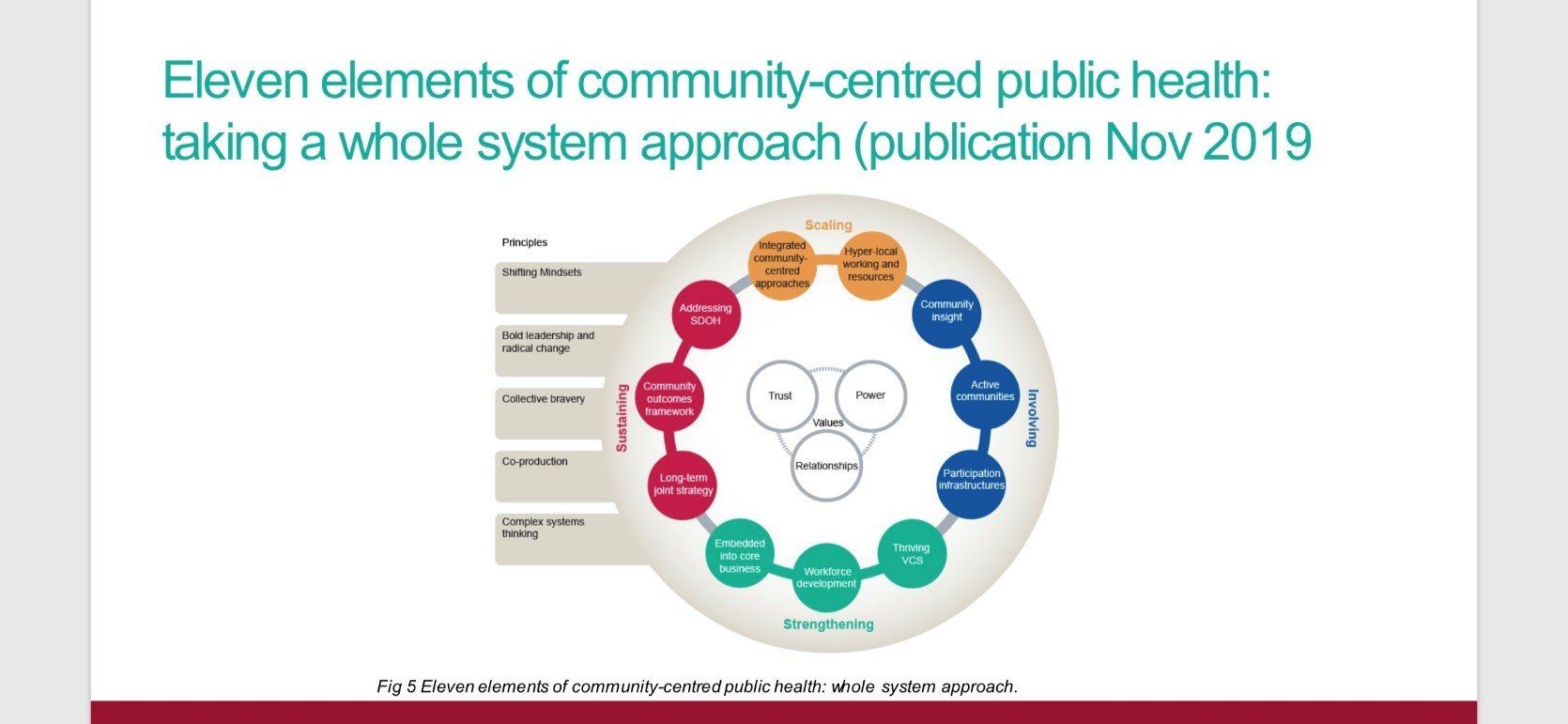
Hot off the press! (well almost) is Jane’s announcement that Public Health England’s new publication for November 2019 on taking a whole system approach to community-centred public health.
For more detail on the topics covered in Jane’s talk visit:
Next up was Tony Cooke, Chief Officer at Leeds Health Partnership Team.
Tony was a talking point for much of the event as he married the theory and research of community work with the reality and outcomes for people in communities. With a focus on how socioeconomic and structural issues adversely impact the health of children and adults living in poverty, Tony introduced us to some interesting stats. These included the statistic that, in the area he covers, 1 in 5 children live in poverty and 76,000 households claim at least one welfare benefit. Therefore, the focus needed to be in improving the health of the poorest the fastest. Therefore, Leeds started to look at those in ‘isolated areas’ moving these areas out of adverse inequalities.
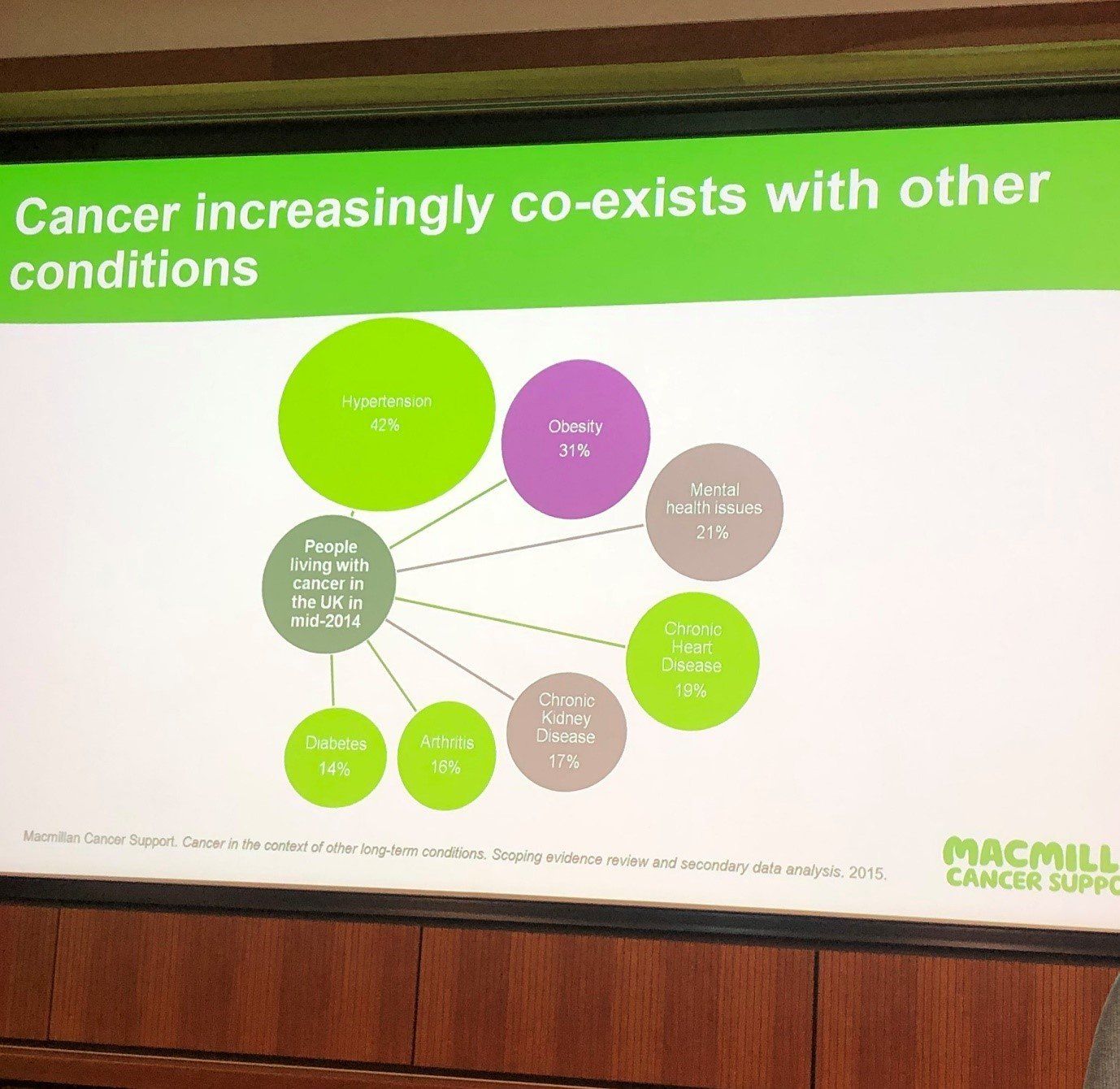
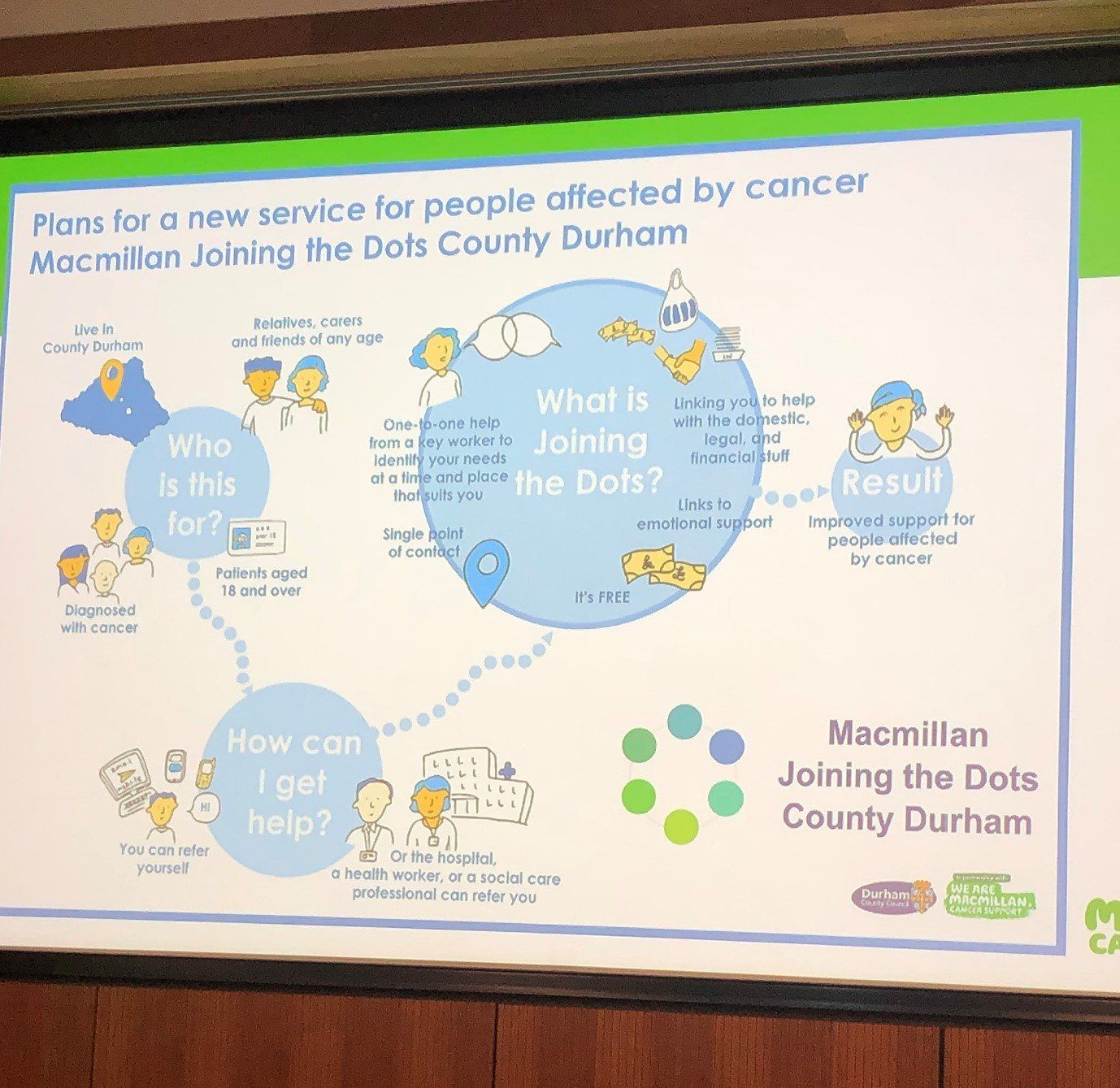
Fiona Flowers at Macmillan Local Area Partnership Programme (MLAPP)
Fiona introduced us to the way the MLAPP had driven coproduction in linking health and Clinical Commissioning Groups (CCGs). There were some fantastic examples here of coproduction and how to start, continue and complete coproductive ways of working such as:
- Coproduction working groups where all the professionals involved had to report to a coproduction governing group with experts by experience.
- Job specification and agreed ways of working coproductively within the group including terms of reference
- Mentoring facilitators
Zereen Rahman-Jennings continued this theme with a presentation on the work carried out by Tower Hamlet's Living with Cancer Programme with examples of how services were changed. See a YouTube video of a previous talk she did here. Zereen valued the benefits of mapping which assets there are within the community and how they interact. She surmised that coproduction can be messy. Her attempts to create a coproduction group initially resulted in an inability to get the same people in the same room on a regular basis to coproduce the project. She revealed that there is more success to be had with more informal processes of gathering interested individuals to develop.
One of the most interesting talks was by Ken Kanu. Ken is the Director of Help On Your Doorstep, an organisation aiming to improve the health and well-being of isolated people in Islington. For Ken, ‘the community is in a better situation to deliver services’. Through their ‘Good Neighbour Scheme’ (GNS) which was ‘hyperlocal’, co-ordinated by paid community workers and included resident involvement produced outcomes such as:
- 82% of people feeling happier, people feeling more connected and closer to others
- 79% felt their health had improved and
- 74% felt more connected with their neighbours.
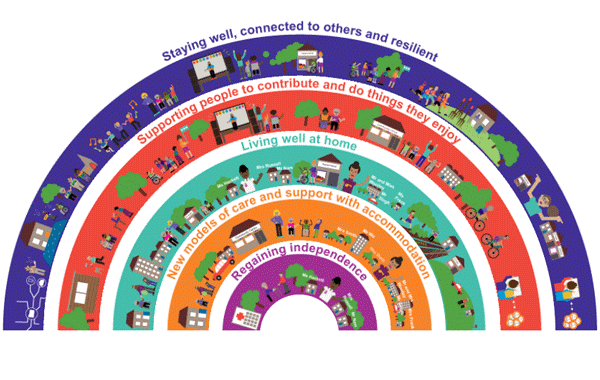
During the afternoon workshop, we heard from Alex Fox from Shared Lives Plus, an organisation which supports people to care for people with care needs in their own homes. Alex revealed the important work TLAP
was doing around promoting coproduction, something they describe as shared living. He also posited a new way of empowering communities by switching the way power dynamics in service delivery are funded and provided to the community that needs support, rather than the top-down external services. He signalled to the work carried out by TLAP (Think Local Act Personal) in their rainbow diagram. Access this dynamic tool and understand who has signed up to and is using it here.
Alex shared that his new book ‘A New Health and Care System’ sets out an original alternative to the current care and health services systems with examples of how the Shared Lives model provides both humanity and care on a sustainable and scalable level.
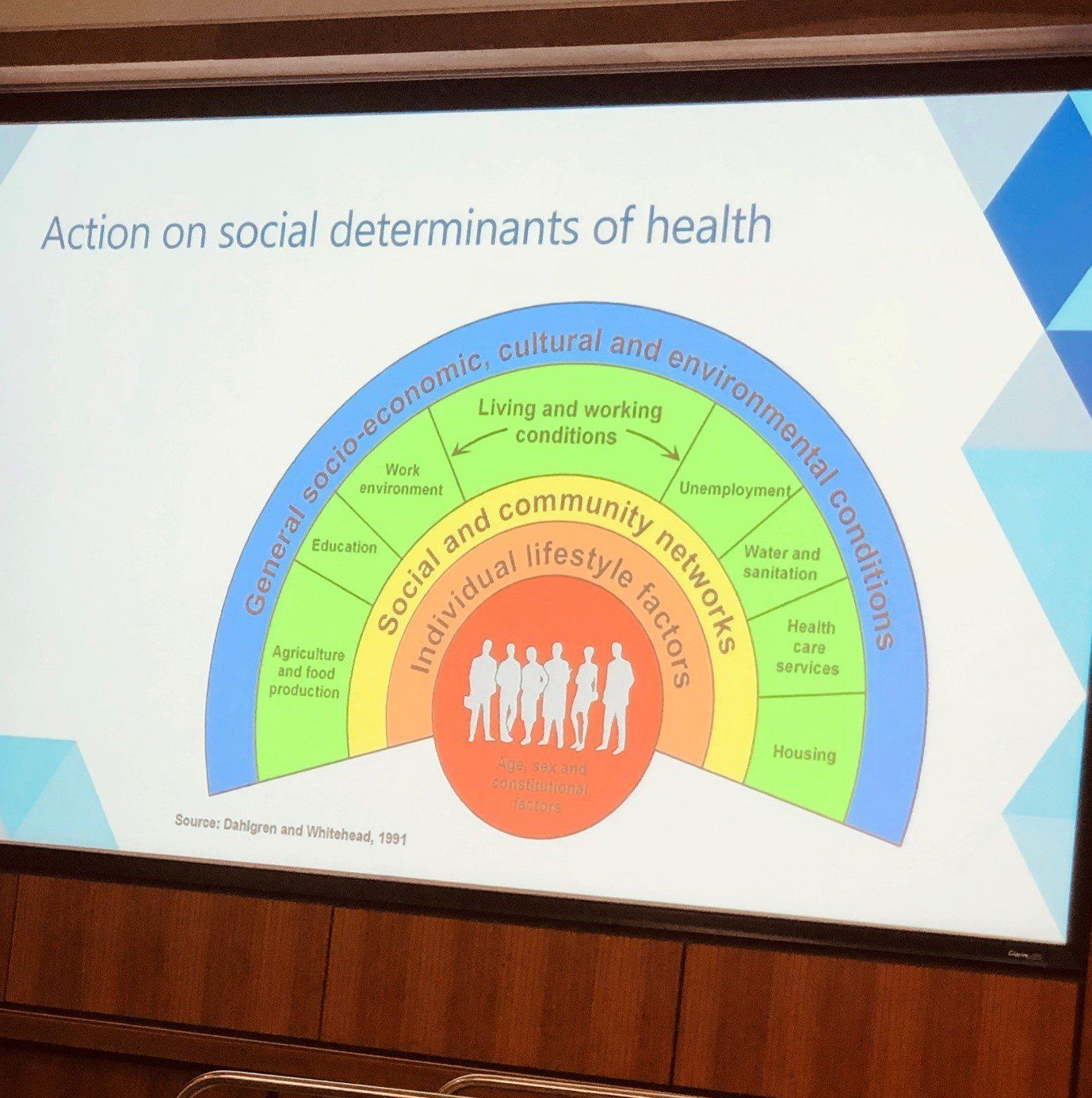
Later, Kathy Martin, Strategic Impact Manager from Northern Ireland Community Development and Health Network, shared the importance of taking action on the social determinants of health.
Her work included supporting people across all of the determinants below, with a focus on pharmacy. Her work recognised the community standing of pharmacists and the network’s funding supported pharmacists to come away from the shop floor and into the community to work.
One of the final talks included messages from Ingrid Abreu Sherer, a Well-being and Civil Society Lead on, of course, well-being and Dr Tim Chadborn (head of behavioural insights at Public Health England) on the benefits of considering behaviours in health and social care.
Ingrid shared some insights, including some well-recognised information that childhood experiences, health and financial security are key determinants of well-being. She also enlightened the room with her take on how well-being changes over time, with middle age showing a key dip in life satisfaction.
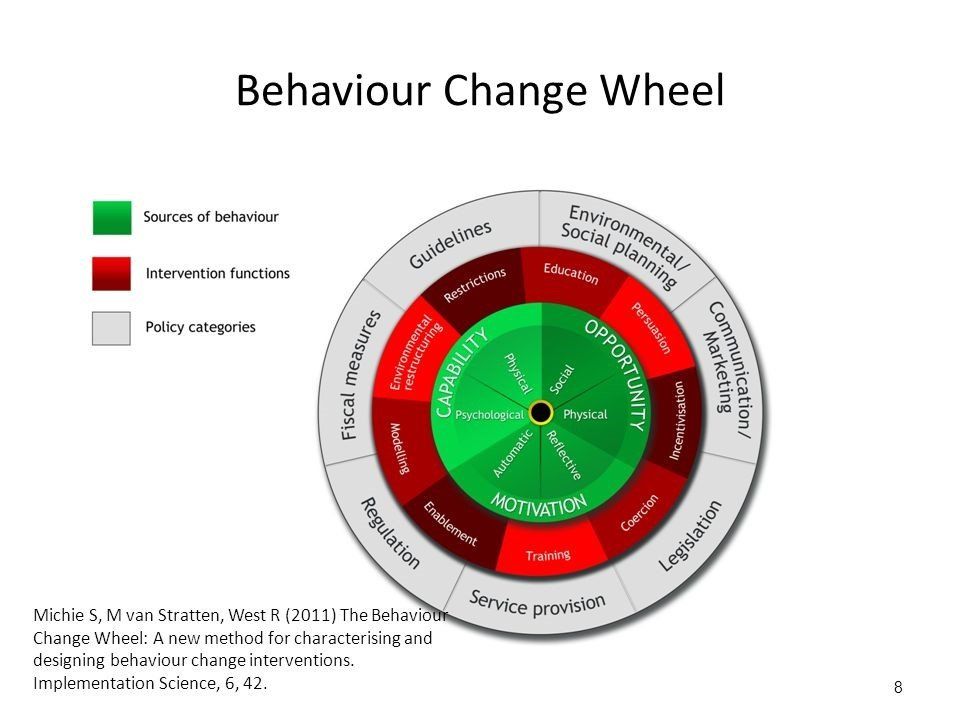
Dr Tim Chadborn encouraged us to consider the myriad of actors within health and social care relationships and how their behaviours will be different across the system, such as volunteers, organisations and systems and how these may or may not contribute to improved social support. He introduced the idea of doing systems thinking from a behavioural perspective.
Snooping
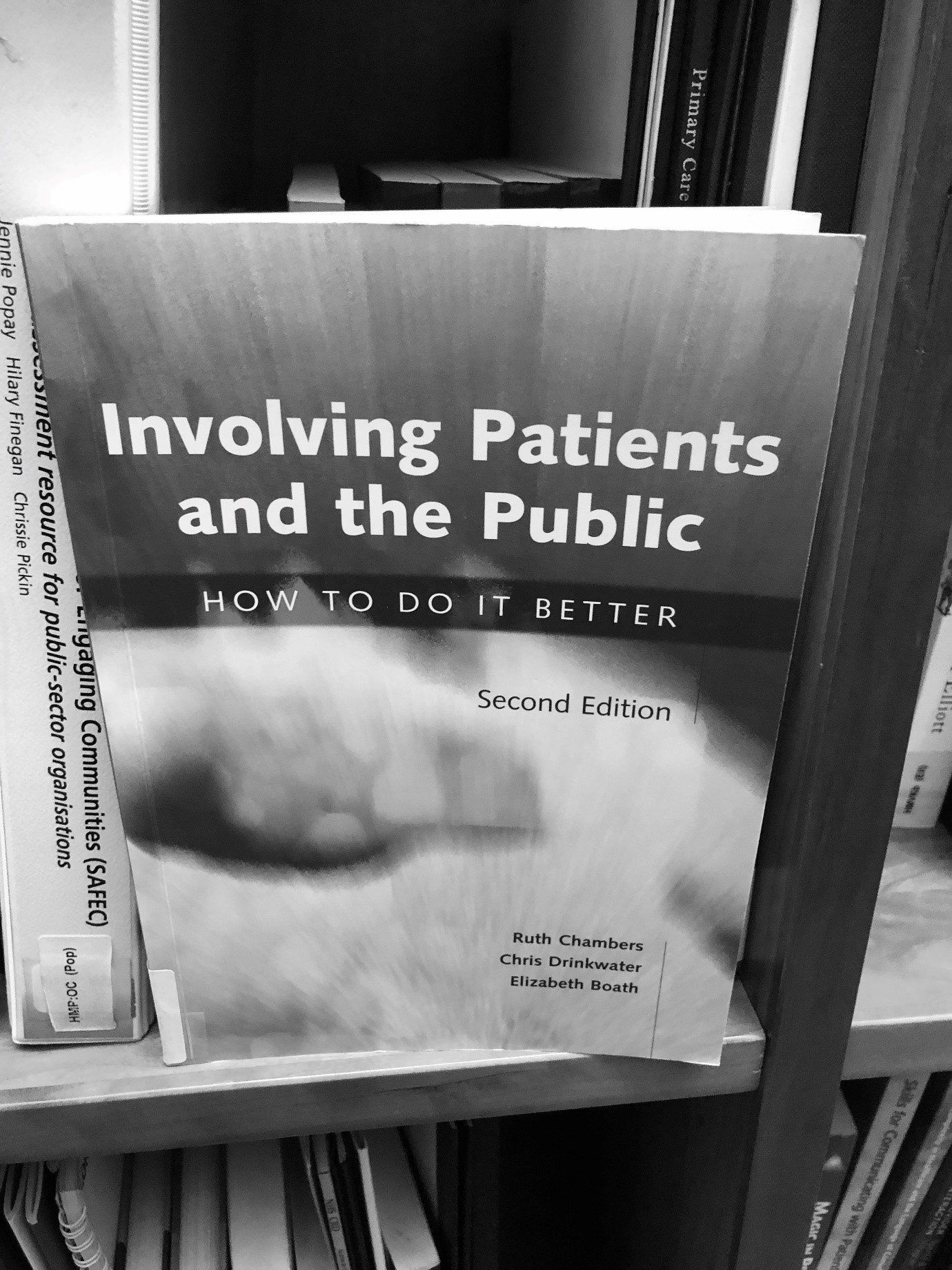
We couldn’t help ourselves but to snoop around The King’s Fund library during our break. It turns out it’s pretty extensive – as you’d expect from a think-tank. Interestingly, we stumbled upon a book on patient involvement from back in 2003. It turns out coproduction and involvement really isn’t that new after all!
Overall, a fantastically informative day and as always, a wealth of information. Check out their website for more on The King’s Fund events, blogs
and publications. Their events come at a cost, but any which we attend, we will blog / tweet as always, for knowledge share and (of course) to open up the care debate!
Comment below in anything you found interesting in this conference summary and as usual feel free to share.
This Facebook widget is no longer supported.
Join us
We will be relying on a small but dedicated team and volunteers.
So, if you would like to be involved, please get in touch at hi@coproducecare.com
and help us open up the care debate, properly democratise care and please do join and share Coproduce Care:
Spread the word and uncover the hidden opportunities for people-led coproduced care
Recent Posts

We are pleased to provide an update our involvement in new projects currently being undertaken by Coproduce Care (CIC) in collaboration with Care and Support West. We will be contributing to local initiatives in Social Care Workforce Redesign, and we are excited to share the project with you. This project is running from June 2023 to June 2024. We will be working on three areas for the next 10 months all in the BNSSG region which are as follows: 1: Investigation of the Trusted Assessor Approach in Health and Social Care Systems In this project, we are investigating the Trusted Assessor Approach in health and social care systems. The objective is to demonstrate the value of Trusted Assessors in streamlining care needs assessment, while also addressing data protection and consent concerns. Case studies will be created from local regions that have implemented this approach, to provide insights into the benefits of Trusted Assessors of reducing delays in accessing required care. 2: BNSSG Opportunities for Levy Sharing and Increasing Apprenticeships in Social Care This project aims to identify opportunities for levy sharing in social care and increase the use of apprenticeships. The project will engage social care providers, training organizations, authorities, and other stakeholders to develop strategies, guidelines, and an implementation plan for utilizing the levy effectively and increasing the use of apprenticeships. 3: Integrated Health and Social Care: Enhancing Collaboration, Improving Quality, Shaping Models of Care, and the Future Social Care Workforce In this project, we are evidencing the enhanced collaboration between social care providers, health services, and local authorities. By mapping existing interfaces and collaborations, we seek to identify opportunities for cross-system benefits and improved outcomes, creating recommendations for integration for BNSSG. Our research will provide valuable insights to integration and collaboration between social care and health. At Coproduce Care (CIC), we believe that collaboration and innovation are vital for transforming social care. Through these projects, we aim to contribute to a more efficient and compassionate system. We extend our gratitude to all stakeholders, providers, commissioners, and policymakers for their invaluable support. Thank you for your continued interest in our endeavours. We will keep you updated as the projects progresses! In the meantime, if you are doing any work in any of these key areas, please get in touch with us using the below form. Thank you!

Dear Thérèse Coffey, We wish you the best of luck on your appointment as Secretary of State for Health and Social Care. Coproduce Care (CIC) is a non-profit organisation set up to democratise the social care debate. We support the voices of those working and involved in social care to influence wider decision making in the sector. Through our continued work in this area, we are writing to address some of the urgent needs of our social care workforce. We welcome your plans to set out ‘ Our plans for patients ’ to ensure our population have easier access to NHS and social care services through winter, putting the needs of patients as priority. To ensure we prioritise the health and wellbeing of our populations, and deliver the best, high-quality care possible, we need to ensure we prioritise the needs of our workforce who are at the front of delivering health and social care . To ensure both the health and wellbeing of our population and our social care workforce, we recommend the following: 1. Improving pay for social care workers, in real terms The Kings Fund published a report which compared the pay of social care workers to ten of the largest supermarkets. It found that nine out of ten supermarkets paid more than most social care roles. An example used is that if care worker left their role for a supermarket position at Tesco, they would see a 6.3% pay increase instantly. We have conducted many surveys, webinars, and connected with our audience on what is crucial to improving care workers working conditions and we have found that increasing pay is consistently the most crucial factor in reflecting the value of the work and high stress and responsibilities of the role . With the current cost of living crisis, this need for increasing pay is only getting more urgent. The sector currently has 100,000 vacancies , with extremely high levels of staff shortages. This affects the capacity to deliver services and the quality of care provided . Providers are struggling to recruit staff as they are competing with supermarkets and hospitality, sectors of which offer less stress and responsibility and more pay. We believe care workers are an invaluable part of our society and therefore should be paid accordingly. We recommend: · Introduce national pay scales that ensure care workers meet a real national living wage as a minimum . This will recognise the full contribution of social care workers make to the health of our population, and that their contribution is a real investment into our population. By increasing pay, we further increase recruitment and retention in the sector, and improve the perception of social care being a highly valuable and promising career choice. · Facilitate efforts to develop appropriate distribution of funds. Ensuring the integration and professionalisation of care is fully realised will allow better distribution of funds resulting in higher wages which better reflects the level of skill, qualifications, responsibilities and selflessness required to work within this sector. 2. Professionalising the care system Health and social care should be professionalised to encourage staff retention, career progression and further skill development. Professionalising care work would ensure that those working in the sector are valued and are provided with the necessary tools to provide high quality care. Currently, there is no accredited qualification for social care workers, without a standardised training process. We hosted a live stream with Gillian Keegan , who mentioned the government’s intention to create a voluntary digital care workforce hub, as well as a skill passport for all Health & Social Care workers. This is understood to allow easier identification of the workforce, including the possibility to share resources and opportunities to encourage the workforce to up-skill and develop. The skills passport would help keep track of the skills care workers have demonstrated over time, meaning career progression would be easier to identify . Whilst individual action is very important, to improve the quality of care, we urge for a standardised career and training development program for all care staff that results in an accredited qualification . We recommend: · Adequate pay to restore and recognise social care work as a valued profession . Extensive skills are involved in care work, and if standardised training and qualifications are implemented, security of applicable income is appropriate to these expectations. By increasing pay, care work has higher professional footing as a recognised career and role. · Ensuring the integration of social care is fully realised . The high fragmentation of the care sector and its lack of integration with NHS services makes it challenging to implement standardised training . The governments white paper ‘ Health and social care integration: joining up care for people, places and population ’ seeks the ambition to join up social care services. We welcome this white paper and its integration policy to achieve higher quality of care and better health outcomes. This ambition requires effort and commitment to the integration at all levels, and we hope that as health secretary, fully putting this policy into practice and reaching its scope, goals, and purpose is your focus in your new role. · Implementing standardised training, improved learning outcomes for workers, including IT, literacy, and numeracy training are addressed with sensitivity and with the voices of the workers at heart . Implementing standardised training would ensure a level of professionalism across the sector, however, must go in line with the security of increased income and security of hours of work. We must protect the wellbeing of our workforce, of which is already experiencing burn-out and exhaustion from the high pressures the sector is facing. We cannot have higher expectations of our workers undertaking standardised training without adequate pay . We hope you agree with our recommendations and seek to ensure we continue to improve the working conditions for our social care workforce. We hope that within your post as the new Health and Social Care Secretary, you prioritise the voices of those most impacted by decision making regarding the sector. Thank you for taking the time to read this letter, CoProduce Care Written by: Gabriella Neal